When I got the news that I had gestational diabetes, it was another worry I didn’t need. I was already carrying a high-risk pregnancy and battling the stresses of having low PAPP-A trying to grow a healthy baby.
Accepting this reality was difficult for me, as was the experience on my physical, mental, and emotional health and well-being.
There were many ups and downs along the way, but I learned to manage gestational diabetes, and created more ups than downs. Eventually, I got through pregnancy and the birth of our son okay.
He was born 6lb 5oz at 38.5 weeks through natural birth, which was thankfully free of complications.
Here’s a glimpse into a typical day living with gestational diabetes and my top tips.

Read, record & share your blood sugar levels regularly
Reading and recording my blood sugar levels and what I ate daily in a schedule kept me in check.
Like my carer’s schedule, I used Google Sheets to keep my recordings online and fully accessible.
I loved Google Sheets for this reason. So convenient to use, I made easy updates 6 times a day on my mobile phone via the cloud. Twice in the morning, twice around lunchtime, and twice in the evening.
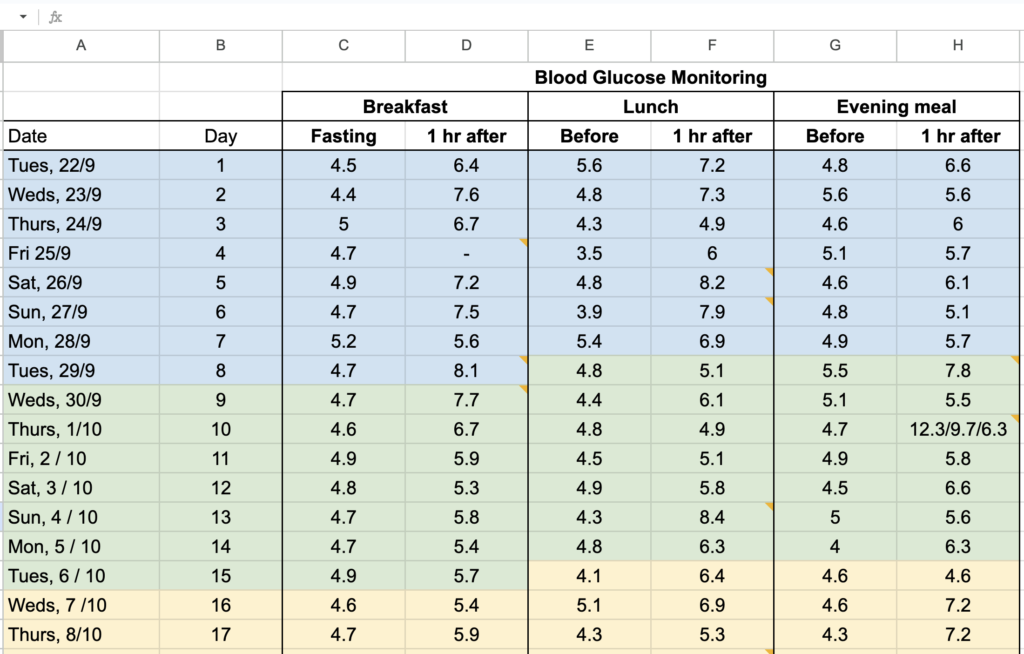
As well as recording my blood sugar readings, I added comments and notes (yellow flags in individual cells) to keep track of the foods that lead to spikes!
This helped me avoid eating similar meals again and gave my gestational diabetes nurse/dietician an honest account of my progress.
I knew I had to do this well (without cheating!) and work with my nurse, using her advice, to keep me and baby safe. So, a schedule like this helped me enormously with the task at hand.
One of my highest readings on Sat, 26/9, resulted from celeriac soup, focaccia bread, mozzarella, and olives. I knew not to have this meal again, to avoid another 8.2 reading and discussed alternatives with my nurse.
Review your stats often with your gestational diabetes nurse/dietician
To keep you and your baby safe and well, use a schedule and review it regularly with your gestational diabetes nurse/dietician. I recorded daily and sent my stats to the nurse every week. This was followed up with weekly appointments to discuss bad days and recipe ideas.
It was invaluable for me to have an expert ‘friend’ give knowledgeable advice. Someone who guided me along the way and gave professional insights about how well I was doing and what I could improve.
Reviewing my stats and progress regularly with my dietician nurse improved my physical, mental, and emotional well-being. Especially on days when readings were off the chart!
On these occasions, I would be told where I’m going right and where things can improve.
I would get advice and reminders to go for:
- 15-20 grams of carbs at breakfast (e.g., 1 x toast)
- 30-40 grams of carbs at lunch or dinner (e.g., closed fist size of pasta or 5 new potatoes)
- Blueberries with half a cup of plain Greek yogurt (breakfast or snack)
- Raw oats porridge (e.g., Quaker original 15-20g) with almonds and coconut flakes
- Semi-skimmed milk with low-fat/sugar hot chocolate (snack or dessert)

Monitor your baby regularly
Every day of my pregnancy, I paid close attention to my baby’s movements, kicks, and punches. I would also regularly ask my husband to listen for the baby’s heartbeat through the belly.
On the one occasion I thought I hadn’t felt movement for a considerable time, I called the midwifery helpline. After a detailed telephone assessment and an informative conversation with a friendly and knowledgeable midwife, I felt reassured everything was okay. Shortly after the call, I had the pleasure of feeling the usual somersaults in the belly again.
Because I had gestational diabetes, low PAPP-A, and high-risk pregnancy, I got more growth scans and hospital review meetings than usual. I attended every appointment, asked many questions, took time to understand reports, requested second opinions, and took on board all advice.
When you have gestational diabetes, it’s natural to do all you can to do the right things to keep you, your baby, and your pregnancy safe and well. Regularly monitoring your baby helps with this.
Lean on your support network
Although I found my conditions and the experience of managing them a real challenge, I got through them by leaning on my support network.
I did this daily and leaned on my husband, sisters, Mum, and closest friends. Professionally, I gained strength from the midwifery team, gestational diabetes nurse/dietician, senior consultants, and sonographers.
By being open, connecting daily, and asking for help, my network helped me immensely to navigate day-to-day challenges.
My husband followed the advice and cooked delicious and nutritious meals for me. My sisters and Mum provided mental and emotional resilience by sharing their pregnancy and birthing stories. Close friends suggested products and activities that worked for them during difficult moments in pregnancy.
I chatted with my support network, shared worries and anxious thoughts, laughed, and gained valuable tips and advice. Through them, I managed my high-risk pregnancy and released cortisol, the stress hormone, to rebalance my sense of well-being.
Exercise and be mindful
I was advised to exercise to help me manage gestational diabetes by reducing my glucose levels. More than this, exercise during lockdown really helped my mental and emotional well-being.
Up until two weeks before my due date, I walked daily with my husband. We explored our local neighbourhood and found places, parks, footpaths, and woodlands we’d never seen nor been to before.
On these long walks, we got mindful, soaking in nature and wildlife while discussing the practicalities of pregnancy and gestational diabetes, including what we’d eat for lunch/dinner. We also anticipated and talked about what parenthood would be like and our favourite boys’ and girls’ names.
Physically, it was good to walk every day and stretch my legs between work or after sitting behind a computer screen at home all day. As someone who’s suffered sciatica, I didn’t want it to rear its ugly head again. So, I was happy to indulge in daily walks to maximise its benefits.

Rest, sleep & do fun enjoyable things
During this challenging period of managing a high-risk pregnancy in lockdown, where stress levels heightened, I did my best to rest and sleep well on a daily basis.
Every night, I followed a relaxing skincare routine and got into bed earlier than usual. It was my way of relieving stress and anxiety hormones, otherwise known as cortisol, from the mind and body.
Read this blog to see why an optimum 8 hours is needed and how our brain flushes out stress toxins during our sleep cycle.
Similarly, having fun and enjoying things that I love made me happier, more positive, and optimistic during a stressful high-risk pregnancy.
Check this for inspiration if you’re looking for some feel-good things to do.
Explore new recipes
My diet didn’t consist of new recipes – just lots of the same meals, which I loved eating, and kept my blood sugar levels low!
I had two favourites. The first was roast chicken with garlic, served with a few boiled new potatoes, carrots, and kale, drenched in chicken/onion gravy. The second was pan-friend salmon with quinoa, fresh cherry tomatoes, avocado, olive oil, and sometimes a fried organic egg on top.
I did miss dessert, though, and often craved a jam doughnut or chocolate cake, which I couldn’t have. Instead, I made do with semi-skimmed milk hot chocolate with low-fat/sugar powder.
For new recipes, Gestational Diabetes UK looks good.
Keep hydrated, drink water, flush out sugar
During my gestational diabetes journey, I learned that drinking water helps the kidneys flush out excess sugar and control glucose levels.
In addition, I read that water contains no carbohydrates or calories, meaning it’s perfect for pregnancy and gestational diabetes!
With water becoming my superpower, I did my best to drink a large glass of water with every meal and another glass between meals.
This approach seemed to work and helped keep my glucose levels stable.
Overall, I hope my top tips for living with and managing gestational diabetes helps you.
Take care, from a carer to other carers x



